About
Professor Bhik Kotecha
Background
Professor Bhik Kotecha was born in Kenya and moved to England in 1972. He grew up in Stanmore and attended Copland High School in Wembley, Middlesex. Following his ambition to study medicine he attended the University of Wales, College of Medicine in Cardiff and qualified in 1984.
He began his surgical career as a surgical house officer with a professorial unit in Cardiff and has many positions including Registrar in Otolaryngology at Hope Hospital / Royal Manchester Children’s Hospital, University of Manchester School of Medicine and Senior Registrar in ENT at The Royal National Throat, Nose and Ear Hospital, London.
Special Interest
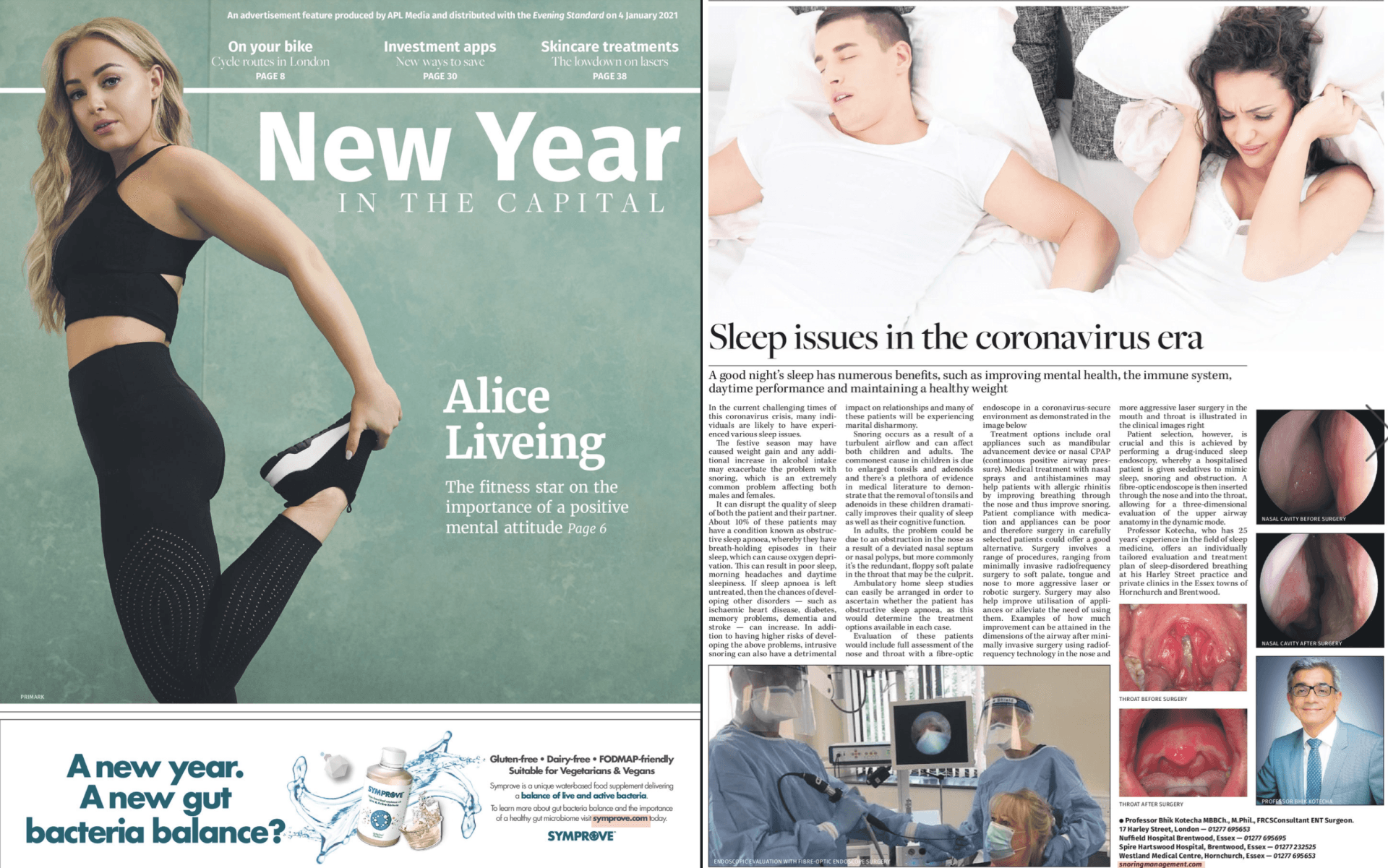
Professor Kotecha’s special interest is in the management of snoring and obstructive sleep apnoea.
Sleep medicine is a relatively new field and has, to date, received very little attention. In order to heighten awareness of problems that patients face with snoring and obstructive sleep apnoea, he has appeared on BBC Breakfast, BBC World, Anglian TV, The Discovery Channel, GMTV and BBC Radio 4. In addition he has also featured within The Daily Mail.
Professor Kotecha also lectures nationally and internationally on the subject and in 2004, he and his team at the Royal National Throat, Nose and Ear Hospital, London won the Hospital Doctor award in the category of ‘Sleep Medicine Team of the Year’.
Qualifications
Prizes & Awards
- July 1984 – D.J. Harries Prize in Surgery
- July 1984 – Block Prize in Respiratory Medicine
- July 1991 – Gold Medal – British Academic Conference, Dublin
- October 1992 – TWJ Fellowship to Beziers, France
- October 1993 – Prize for best presentation 17th International Conference of Young Otorhinolaryngologist, St. Petersburg, Russia
- November 2002 – Finalist Hospital Doctor Team of the Year Award – Sleep Medicine Section
- July 2003 – First Prize Barking Havering and Redbridge Trust Innovation Award Scheme funded by NHS Modernisation Agency
- November 2004 – Winner of Hospital Doctor Team of the Year Award – Sleep Medicine Section (Read more)
National Award
Sleep Medicine Team of the Year
Awarded by Hospital DoctorAt least 45% of the adult population snore regularly and loud enough to disturb those around them.
Teaching
Professor Kotecha has enjoyed teaching from very early on in his career.
As a demonstrator in anatomy at the University of Liverpool, he used to teach anatomy to medical and dental students. As a Consultant, he actively participated in teaching and training SHOs and SpRs.
He was actively involved in various teaching sessions at the Royal College of Surgeons of England and on the Intercollegiate Fellowship Course at the Institute of Otology and Laryngology.
On a regular basis, he used to organise and lecture at the Snoring and Sleep Disorder Course, which was held at the Royal National Throat, Nose and Ear Hospital.
He has been a clinical examiner for the British Association of Audiological Technicians and is an Honorary Senior Lecturer at the Institute of Otology and Laryngology, University College of London.
Prof Kotecha has over one hundred presentations & publications, with the majority being on sleep related breathing disorders. His publications include 2 text books, 9 chapters and numerous peer reviewed articles.
The three top would include:
- A retrospective audit on 2485 patients undergoing drug induced sedation endoscopy, as this is the largest reported audit on this topic in the world.
- A review article on surgery in adult OSA in a Sleep Medicine Reviews Journal with an impact factor of 9.
- Kotecha technique of laser palatoplasty, as this was my personal contribution in innovating a new modification of previously aggressive and radical technique thus reducing overall morbidity associated with previous techniques.
According to Research gate data, there have been more than 2000 downloads of his published articles, more than 1800 citations and 6000 profile views resulting in an overall 117.92 Impact points attained. A full list is provided below.
Prof Kotecha has also recently written articles in the Daily Mail and Mail on Sunday which can be found here: Mail on Sunday
Daily Mail.
"A novel non-surgical treatment for snoring' article in Healthcare Innovations
features Prof Kotecha.
At least 45% of the adult population snore regularly and loud enough to disturb those around them.
Sleep Issues in the Coronavirus Era
At least 45% of the adult population snore regularly and loud enough to disturb those around them.
ENT - COVID19
Professor Bhik Kotecha was invited to the 'Healing our Earth' global Online Session to share some extremely useful and detailed insight regarding the health of our ear, nose and throat during the Covid19 pandemic
Patient Testimonials
SUSAN AND JOSEPH
In this video Susan talks about her son Joseph who suffered with persistent tonsil problems leading to numerous absences from school.
Prof Kotecha assessed and treated Joseph enabling him to have a speedy recovery and no longer suffer with tonsillitis.
Read more about throat conditions here from the ENTUK website.
EILEEN AND JAMES
In this video Eillen talks about her husband James who regularly kept Eileen awake at night with his loud snoring. James also talks about how he felt constantly tired during the day affecting the way he functioned.
James was diagnosed with obstructive sleep apnoea and after trying various unsuccessful treatments he was referred to Prof Kotecha. After careful assessment and counselling he opted to undergo surgery giving instant and tremendous results.
Read more about snoring and obstructive sleep apnoea here from the ENTUK website.